James' appetite has doubled after the surgery.
While this is a good thing he is waking up every two hours to eat!!
Mommy is very tired
Thursday, 29 December 2011
Sunday, 25 December 2011
Friday, 16 December 2011
Wednesday, 14 December 2011
A crappy deal
James may want to kill me for sharing this one day, but we all have embarrassing baby stories told about us.
My boy use to be a twice a week pooper, maybe three times if Mommy ate something that didn't agree with James' tummy, but the average was twice a week. He was also really good at holding them in for Daddy.
Well I am not sure what they did to him during surgery but this kid is FILLED with poop!!!
I have had to change more diapers in the last few days then I did in almost a month!!
It also lead to this phone conversation after Mark had James on his lap and then passed him over to me so he could go out
Me: Hey, um look down
Mark: Why??
Me: Well, I'm covered in Poop just wonder if you are too?
Pause:
Mark: Ah CRAP!!!
My boy use to be a twice a week pooper, maybe three times if Mommy ate something that didn't agree with James' tummy, but the average was twice a week. He was also really good at holding them in for Daddy.
Well I am not sure what they did to him during surgery but this kid is FILLED with poop!!!
I have had to change more diapers in the last few days then I did in almost a month!!
It also lead to this phone conversation after Mark had James on his lap and then passed him over to me so he could go out
Me: Hey, um look down
Mark: Why??
Me: Well, I'm covered in Poop just wonder if you are too?
Pause:
Mark: Ah CRAP!!!
Friday, 9 December 2011
One more hurdle
We have one more hurdle to get over to go home. James just needs a Echocardiogram and we can go home as long as it looks good!!
Hopefully we will be home by dinner
Hopefully we will be home by dinner
One more thing gone!!!
They just removed James' heart monitor. It should have come off last night but he was mesmerized by the screen so we left it on.
This only leaves his oxygen monitor and drainage tubes.
He is WIDE awake....it is 4:30 a.m. Mommy is not happy
This only leaves his oxygen monitor and drainage tubes.
He is WIDE awake....it is 4:30 a.m. Mommy is not happy
Wednesday, 7 December 2011
Day Zero
This is my story of the first 24 hours or as it is called at HSC, Day 0. It is a bit long and detailed. In some parts it also gets a little graphic. Here goes.
So we arrived early at HSC and by early I mean before six am early. I knew something was up, but everyone that met me was so nice. They weighted me and took my vitals and measured me and so on. I was getting really hungry but all they gave me was a small bit of sugar water.
At 0730 we went over to the pre op area. There were alot of crying children. Now I was really wondering what was going on. My fears were put to rest as a beautiful young nurse came over and played with me. She was so nice. Mommy and Daddy look sad. I don't know why. The nice nurse and I were going somewhere. I was off to an adventure!!!!
I was put on a bed and more people came over to play with me, including a real nice man I met in pre op. He said he was with anastasia. I don't know what that is but it sounds pretty cool! Before I knew it there was a mask over my face and I guess I fell asleep.
From here on I'm going by what Daddy told me. It is kind of detailed to appease the medical people that are reading this. After I went to sleep I was intubated with a cuffed 3.0 tube (this is important later). Then they proceeded to put an arterial line in my neck, two IVs, a urinary catheter, an NG tube and monitored me with various other devices. They made an incision in my chest, cut through my sternum and gained access to my heart. I was hooked up to a heart lung bypass machine where i took one unit if blood. This was because I weighed in at 6 kgs. My body wouldnt be able to lcirculate enough blood to keep my organs alive. Once that was set up and running well, the surgeons began the repair of my TOF. They patched the VSD (ventricular septal defect) and a tiny ASD (atrial septal defect). Then they inspected cusps of my valves for my pulmonary artery. Although they aren't perfect they are "acceptable". Luckily they didn't have to do a valve replacement. In the future that might change, but for now the valves aren't leaking. The surgeon also said my pulmonary artery is narrow, but that may change as I grow up. To finish up the surgery they took me off the heart lung bypass to make sure everything was on the up and up. They also placed pacing wires directly on my heart incase I suffered a bout of bradycardia or some kind of bradydisrhythmia. Two wires remain hanging out of my incision and should be removed when I go to 4D. Two chest tubes where also placed to allow blood to drain from my chest cavity. Wow what a morning. I'm glad I was asleep for that!!!
At 12:00 The surgeon came out to tell Mommy and Daddy that I was doing well. They were very relieved. Now they had to wait for one hour to see me in the CCU. What an eternity it was for them.
Finaly at 13:10 Mommy and Daddy were taken to see me. I was heavily sedated, hooked up to the vent which was breathing for me. I had heparin, plavix, morphine, and antibiotics running through pumps. My urinary catheter was draining well and so was my chest tubes, although the blood from my chest was quite dark and thick.
My blood pressure and heart rate were a bit high. My blood pressure was 124/56 and my heart rate was 176. I was satting very well, but my Etco2 was quite high. In the high 60s and low 70s to ne exact. My blood work was showing I was a bit acidotic. On top of this some gunk was in my lungs. They suctioned me but because I was intubated with a small 3.0 endotracheal tube, they couldn't get it out. They decided to take the tube out and re intubated me with a 3.5 tube. I was re sedated as I was able to open my eyes a bit and squeeze mommy and daddy's fingers. A 3.5 uncuffed tube was placed with no problem. Unfortunately there was a large leak. I started to blow bubbles out of my mouth and other nostril! So after some discussion with respiratory and the attending doctor I was again intubated with a larger 4.0 tube. That helped because they could suction the crap out of my lungs, and it was tight enough that there wasn't much of a leak around the tube. My Etco2 then dropped to the low fifties, witch is better but still not great.
During this time my blood pressure took a tumble to 68/48 and my pulse remained at 170. The decision was made that I might be volume deprived. An order for an albumin infusion was ordered and started. For those that don't know, albumin is a blood product. Within a fairly short time, my blood pressure was up to a respectable 90/54 and my pulse was dropping to around 140. It was working nice. My Etco2 was a near perfect 41mm/mg! I was making progress. The sedative was starting to wear off so I was able to grab mommy and daddy's fingers again and I would move my toes if someone tickled them. I was also trying to suck, so mommy put a soother in my mouth. The RT started to wean me off my vent. This was a slow process that took all night. Blood gasses were taken from my arterial line every few hours to make sure the drugs and ventilation support was working in harmony. I really started to arouse around midnight. I tried to do my usual wake up smile, but something was very wrong. My whole body hurt. I started to cry but nothing would come out !!!! What the hell???
The doctor and the RT started to debate the pros and cons of sedating me yet again. It turns out they did two intubations in the OR not one, so that ment I had been intubated 4 times in 12 hours. Luckily the last 2 daddy watched and agreed that they were not traumatic intubations so my airway should be okay. They gave me alot of morphine to control my pain but I was still very upset. I laid on the bed trying to cry but with no success.
Mommy, daddy and the nurses did all they could to keep me calm. At 0330 am Iwas switched from assisted ventilations to CPAP via my tube. What this does is increase the tidal volume in my lungs when I can't do it myself. As my drugs wore off I was getting so agitated I was trying to pull out my endotracheal tube. Jack the RT and daddy had a big discussion with the doctor about getting me extubated ASAP. At 0630 I was extubated by Jack. It hurt but at least I could cry properly.
My throat was so raw and sore. I had a plastic oxygen tent that looked like a space helmet put over my head. My O2 SATs stayed at a beautiful 100%. They repeated my blood gases and before 0900 I was doing great and didn't require any oxygen what so ever. So ended "Day Zero". What a busy day!!!!
So we arrived early at HSC and by early I mean before six am early. I knew something was up, but everyone that met me was so nice. They weighted me and took my vitals and measured me and so on. I was getting really hungry but all they gave me was a small bit of sugar water.
At 0730 we went over to the pre op area. There were alot of crying children. Now I was really wondering what was going on. My fears were put to rest as a beautiful young nurse came over and played with me. She was so nice. Mommy and Daddy look sad. I don't know why. The nice nurse and I were going somewhere. I was off to an adventure!!!!
I was put on a bed and more people came over to play with me, including a real nice man I met in pre op. He said he was with anastasia. I don't know what that is but it sounds pretty cool! Before I knew it there was a mask over my face and I guess I fell asleep.
From here on I'm going by what Daddy told me. It is kind of detailed to appease the medical people that are reading this. After I went to sleep I was intubated with a cuffed 3.0 tube (this is important later). Then they proceeded to put an arterial line in my neck, two IVs, a urinary catheter, an NG tube and monitored me with various other devices. They made an incision in my chest, cut through my sternum and gained access to my heart. I was hooked up to a heart lung bypass machine where i took one unit if blood. This was because I weighed in at 6 kgs. My body wouldnt be able to lcirculate enough blood to keep my organs alive. Once that was set up and running well, the surgeons began the repair of my TOF. They patched the VSD (ventricular septal defect) and a tiny ASD (atrial septal defect). Then they inspected cusps of my valves for my pulmonary artery. Although they aren't perfect they are "acceptable". Luckily they didn't have to do a valve replacement. In the future that might change, but for now the valves aren't leaking. The surgeon also said my pulmonary artery is narrow, but that may change as I grow up. To finish up the surgery they took me off the heart lung bypass to make sure everything was on the up and up. They also placed pacing wires directly on my heart incase I suffered a bout of bradycardia or some kind of bradydisrhythmia. Two wires remain hanging out of my incision and should be removed when I go to 4D. Two chest tubes where also placed to allow blood to drain from my chest cavity. Wow what a morning. I'm glad I was asleep for that!!!
At 12:00 The surgeon came out to tell Mommy and Daddy that I was doing well. They were very relieved. Now they had to wait for one hour to see me in the CCU. What an eternity it was for them.
Finaly at 13:10 Mommy and Daddy were taken to see me. I was heavily sedated, hooked up to the vent which was breathing for me. I had heparin, plavix, morphine, and antibiotics running through pumps. My urinary catheter was draining well and so was my chest tubes, although the blood from my chest was quite dark and thick.
My blood pressure and heart rate were a bit high. My blood pressure was 124/56 and my heart rate was 176. I was satting very well, but my Etco2 was quite high. In the high 60s and low 70s to ne exact. My blood work was showing I was a bit acidotic. On top of this some gunk was in my lungs. They suctioned me but because I was intubated with a small 3.0 endotracheal tube, they couldn't get it out. They decided to take the tube out and re intubated me with a 3.5 tube. I was re sedated as I was able to open my eyes a bit and squeeze mommy and daddy's fingers. A 3.5 uncuffed tube was placed with no problem. Unfortunately there was a large leak. I started to blow bubbles out of my mouth and other nostril! So after some discussion with respiratory and the attending doctor I was again intubated with a larger 4.0 tube. That helped because they could suction the crap out of my lungs, and it was tight enough that there wasn't much of a leak around the tube. My Etco2 then dropped to the low fifties, witch is better but still not great.
During this time my blood pressure took a tumble to 68/48 and my pulse remained at 170. The decision was made that I might be volume deprived. An order for an albumin infusion was ordered and started. For those that don't know, albumin is a blood product. Within a fairly short time, my blood pressure was up to a respectable 90/54 and my pulse was dropping to around 140. It was working nice. My Etco2 was a near perfect 41mm/mg! I was making progress. The sedative was starting to wear off so I was able to grab mommy and daddy's fingers again and I would move my toes if someone tickled them. I was also trying to suck, so mommy put a soother in my mouth. The RT started to wean me off my vent. This was a slow process that took all night. Blood gasses were taken from my arterial line every few hours to make sure the drugs and ventilation support was working in harmony. I really started to arouse around midnight. I tried to do my usual wake up smile, but something was very wrong. My whole body hurt. I started to cry but nothing would come out !!!! What the hell???
The doctor and the RT started to debate the pros and cons of sedating me yet again. It turns out they did two intubations in the OR not one, so that ment I had been intubated 4 times in 12 hours. Luckily the last 2 daddy watched and agreed that they were not traumatic intubations so my airway should be okay. They gave me alot of morphine to control my pain but I was still very upset. I laid on the bed trying to cry but with no success.
Mommy, daddy and the nurses did all they could to keep me calm. At 0330 am Iwas switched from assisted ventilations to CPAP via my tube. What this does is increase the tidal volume in my lungs when I can't do it myself. As my drugs wore off I was getting so agitated I was trying to pull out my endotracheal tube. Jack the RT and daddy had a big discussion with the doctor about getting me extubated ASAP. At 0630 I was extubated by Jack. It hurt but at least I could cry properly.
My throat was so raw and sore. I had a plastic oxygen tent that looked like a space helmet put over my head. My O2 SATs stayed at a beautiful 100%. They repeated my blood gases and before 0900 I was doing great and didn't require any oxygen what so ever. So ended "Day Zero". What a busy day!!!!
Tuesday, 6 December 2011
Monday, 5 December 2011
We got to see him
We got to see James!!
He is still heavily sedated
Mark doesn't want to leave the bedside so it might take a while to get a detailed update.
They are hoping to get the tube out tonight
He is still heavily sedated
Mark doesn't want to leave the bedside so it might take a while to get a detailed update.
They are hoping to get the tube out tonight
He is out of surgery
James I out of surgery
He still has a breathing tube in, hopefully it will come out tonight.
It was the best outcome possible
Thank you all for the prayers and old thoughts. They were heard!!!
He still has a breathing tube in, hopefully it will come out tonight.
It was the best outcome possible
Thank you all for the prayers and old thoughts. They were heard!!!
Gone to surgery
James went down to the OR about 20 minutes ago.
I will be at least 4 hours till we hear anything
He will have to spend at least a few hours in the ICU
I will keep everyone updated
I will be at least 4 hours till we hear anything
He will have to spend at least a few hours in the ICU
I will keep everyone updated
Saturday, 3 December 2011
Friday, 2 December 2011
Tuesday, 29 November 2011
Rough day
Jame is not having a good day today.
Some days you can tell that his little body is working harder to do everything, over all he is just fussy.
His color is not great as well. It is so hard to watch him go through this, as a mommy I just want to make him feel better but I can't.
Thank you for all your love and support you have shown our family already. We are blessed to be surrounded by so many amazing people!!
Some days you can tell that his little body is working harder to do everything, over all he is just fussy.
His color is not great as well. It is so hard to watch him go through this, as a mommy I just want to make him feel better but I can't.
Thank you for all your love and support you have shown our family already. We are blessed to be surrounded by so many amazing people!!
Wednesday, 23 November 2011
James like to share!!!
James has learned how to share already!!
We have a lot of extra breast milk in this household. We have a stockpile in our freezer, and my moms since we ran our of room in ours.
When we had two freezers full of milk I knew I needed to get rid of some of it, but throwing it out seemed like such a waste of such a precious resource. I know of a few babies who are allergic to formula and breast milk was their only option and I wondered what happened to these babies when their mom's couldn't breast feed for whatever reason?
My research brought me to an organization called Human Milk for Human Babies. I connected with my local chapter on Facebook and was then put in touch with local moms and babies looking for milk.
So far I have donated over 300 oz to 2 different babies! I have a small stockpile on hand if something happens and I need it for James, and I am cycling it through, once I double up the stock pile I pass off the milk to one of the families.
If you are like James and I and have some extra breast milk in your freezer, or know someone who does, you might want to consider donating it.
Here are some of the FAQs from The Human Milk for Human Babies Facebook Page
We have a lot of extra breast milk in this household. We have a stockpile in our freezer, and my moms since we ran our of room in ours.
When we had two freezers full of milk I knew I needed to get rid of some of it, but throwing it out seemed like such a waste of such a precious resource. I know of a few babies who are allergic to formula and breast milk was their only option and I wondered what happened to these babies when their mom's couldn't breast feed for whatever reason?
My research brought me to an organization called Human Milk for Human Babies. I connected with my local chapter on Facebook and was then put in touch with local moms and babies looking for milk.
So far I have donated over 300 oz to 2 different babies! I have a small stockpile on hand if something happens and I need it for James, and I am cycling it through, once I double up the stock pile I pass off the milk to one of the families.
If you are like James and I and have some extra breast milk in your freezer, or know someone who does, you might want to consider donating it.
Here are some of the FAQs from The Human Milk for Human Babies Facebook Page
Q: What is the mission of Human Milk 4 Human Babies Global Network?
A: The mission of Human Milk 4 Human Babies Global Network is to promote the nourishment of babies and children around the world with human milk. We are dedicated to fostering community between local families who have chosen to share breastmilk.
Q: What is informed choice?
A: Informed choice is a choice made by competent individuals, free from coercion, that takes into account sufficient information to make a decision. This information should include the benefits and risks of a course of action, as well as taking into account what alternatives are available, and an individual's intuitive feelings on the subject.
Q: How does it work?
A:
* Find your community page on Facebook.
* Post on the Discussion Tab if you would like to donate or receive breast milk.
* Talk to other mothers on the Wall and check for reminders posted there.
* If you see a post from someone who is a potential match for you, contact them directly via private message or on the discussion board. Here are some guidelines for safe social networking.
***It is in the spirit of informed choice that milk sharing on these pages will occur, and all people posting here will take complete responsibility for the outcome of milk sharing.***
Q: What does HM4HB Global NOT do?
A:
* Support or approve of the selling of breastmilk on our network.
* Provide medical advice or clinical care.
* Screen donors or recipients.
* Provide contracts or questionnaires.
* Decide who should receive breastmilk.
* Collect, store or distribute breastmilk.
* Receive money, payment, donations or funding of any kind.
* Reimburse volunteers/supporters.
* Act as mediators or advisors if difficulties or misunderstandings occur between parties.
* Accept liability for the outcomes associated with sharing breastmilk.
* Expect mothers to try to increase their supply in order to donate or receive milk.
Q: What may be expected of me as a donor and/or recipient?
A: Expectations will vary depending on the family shared with and the donor. You can work out the details together until you are satisfied. Openness and honesty is expected, as well as full disclosure, on the part of all parties involved. The principles of informed choice are of utmost importance in the context of peer-to-peer milk sharing.
Q: What if I am unable to reach an agreement with my donor/recipient or I don’t feel comfortable receiving/giving milk?
A: If the recipient does not feel comfortable with their donor, or vice versa, (s)he is under no obligation to participate in milk sharing with that person. Please post on your HM4HB Global chapter to find a more suitable arrangement. HM4HB Global is not responsible for the outcome of any milk sharing arrangements.
Q: What can I do to provide to my baby the safest possible breastmilk?
A: Full disclosure reduces risk. Suggested points of discussion can include medications, alcohol and drug use. In many countries, testing for infectious diseases is done during routine prenatal/antenatal care. You may be able to consult a health care provider to obtain further testing if desired. Some diseases to consider are HIV, hepatitis B and C, syphilis, HTLV, as well as cytomegalovirus (CMV) and tuberculosis. You can ask for copies of those test results.
If you cannot get a complete picture of the health of your donor, one option is to look into at-home pasteurization.
Q: Is it possible to pasteurize breastmilk at home? What pathogens are destroyed by this process?
A: There is a simple, low-tech form of flash pasteurization, called "flash-heating," that can be done on stove-top at home. Research indicates it can destroy a number of pathogens while retaining the greatest amount of beneficial properties of breastmilk when compared with other types of pasteurization. This process can be done by the recipient just prior to feeding the baby. See this straight-forward explanation for a "how-to" on Flash-heating.
Q: How (and for how long) can milk be stored?
A: Expressed milk can be stored in various breastmilk containers following the manufacturers' instructions. Noting the date on the container will make sure it is consumed within a safe time frame. Storage times will vary based on where it is stored. This link gives information on storage.
Q: What can I do to reduce the risk of contamination?
A: Whether you are using hand expression, a pump, or wet nursing, your hands and supplies should be clean and dry, and your breasts should also be clean and free of sores or blisters. Your pump manual will have information about how to properly use and clean your pump. For more information on hand expression technique, see this video. Also, this page may also be useful.
Q: My baby is healthy, can I still ask for donor milk?
A: Absolutely. There does not need to be a medical reason for your baby to have breastmilk. Human milk is for human babies and children. The Global network does not prioritize recipients, but simply offers an online space where families can connect and make informed milk sharing choices. You can ask for milk for your child at any time and for any reason, regardless of age.
Q: My baby is 4 months old, can I receive milk from a donor whose baby is 12 months old?
A: As babies grow and mature, their nutritional needs also change. It is therefore ideal for donor breastmilk to either come from a mother whose baby is around the same age or from a mother who pumped when her baby was around that same age. However, as per the World Health Organization's guidelines, in most circumstances human milk is preferable to milk substitutes, even when there is a difference in age.
Q: Do I have to use a bottle to feed my baby donor milk?
A: No, many mothers use an at-the-breast supplementer to feed their babies. This device includes a container attached to a small feeding tube that is either taped to the breast or placed inside the baby's mouth while the baby is latched onto the breast. This allows the baby to receive the donor milk while still stimulating mother's breast and taking in any milk she is making. While this device can be purchased, you can also make your own. Some families use a small cup, a dental syringe, a spoon or other methods.
A: The mission of Human Milk 4 Human Babies Global Network is to promote the nourishment of babies and children around the world with human milk. We are dedicated to fostering community between local families who have chosen to share breastmilk.
Q: What is informed choice?
A: Informed choice is a choice made by competent individuals, free from coercion, that takes into account sufficient information to make a decision. This information should include the benefits and risks of a course of action, as well as taking into account what alternatives are available, and an individual's intuitive feelings on the subject.
Q: How does it work?
A:
* Find your community page on Facebook.
* Post on the Discussion Tab if you would like to donate or receive breast milk.
* Talk to other mothers on the Wall and check for reminders posted there.
* If you see a post from someone who is a potential match for you, contact them directly via private message or on the discussion board. Here are some guidelines for safe social networking.
***It is in the spirit of informed choice that milk sharing on these pages will occur, and all people posting here will take complete responsibility for the outcome of milk sharing.***
Q: What does HM4HB Global NOT do?
A:
* Support or approve of the selling of breastmilk on our network.
* Provide medical advice or clinical care.
* Screen donors or recipients.
* Provide contracts or questionnaires.
* Decide who should receive breastmilk.
* Collect, store or distribute breastmilk.
* Receive money, payment, donations or funding of any kind.
* Reimburse volunteers/supporters.
* Act as mediators or advisors if difficulties or misunderstandings occur between parties.
* Accept liability for the outcomes associated with sharing breastmilk.
* Expect mothers to try to increase their supply in order to donate or receive milk.
Q: What may be expected of me as a donor and/or recipient?
A: Expectations will vary depending on the family shared with and the donor. You can work out the details together until you are satisfied. Openness and honesty is expected, as well as full disclosure, on the part of all parties involved. The principles of informed choice are of utmost importance in the context of peer-to-peer milk sharing.
Q: What if I am unable to reach an agreement with my donor/recipient or I don’t feel comfortable receiving/giving milk?
A: If the recipient does not feel comfortable with their donor, or vice versa, (s)he is under no obligation to participate in milk sharing with that person. Please post on your HM4HB Global chapter to find a more suitable arrangement. HM4HB Global is not responsible for the outcome of any milk sharing arrangements.
Q: What can I do to provide to my baby the safest possible breastmilk?
A: Full disclosure reduces risk. Suggested points of discussion can include medications, alcohol and drug use. In many countries, testing for infectious diseases is done during routine prenatal/antenatal care. You may be able to consult a health care provider to obtain further testing if desired. Some diseases to consider are HIV, hepatitis B and C, syphilis, HTLV, as well as cytomegalovirus (CMV) and tuberculosis. You can ask for copies of those test results.
If you cannot get a complete picture of the health of your donor, one option is to look into at-home pasteurization.
Q: Is it possible to pasteurize breastmilk at home? What pathogens are destroyed by this process?
A: There is a simple, low-tech form of flash pasteurization, called "flash-heating," that can be done on stove-top at home. Research indicates it can destroy a number of pathogens while retaining the greatest amount of beneficial properties of breastmilk when compared with other types of pasteurization. This process can be done by the recipient just prior to feeding the baby. See this straight-forward explanation for a "how-to" on Flash-heating.
Q: How (and for how long) can milk be stored?
A: Expressed milk can be stored in various breastmilk containers following the manufacturers' instructions. Noting the date on the container will make sure it is consumed within a safe time frame. Storage times will vary based on where it is stored. This link gives information on storage.
Q: What can I do to reduce the risk of contamination?
A: Whether you are using hand expression, a pump, or wet nursing, your hands and supplies should be clean and dry, and your breasts should also be clean and free of sores or blisters. Your pump manual will have information about how to properly use and clean your pump. For more information on hand expression technique, see this video. Also, this page may also be useful.
Q: My baby is healthy, can I still ask for donor milk?
A: Absolutely. There does not need to be a medical reason for your baby to have breastmilk. Human milk is for human babies and children. The Global network does not prioritize recipients, but simply offers an online space where families can connect and make informed milk sharing choices. You can ask for milk for your child at any time and for any reason, regardless of age.
Q: My baby is 4 months old, can I receive milk from a donor whose baby is 12 months old?
A: As babies grow and mature, their nutritional needs also change. It is therefore ideal for donor breastmilk to either come from a mother whose baby is around the same age or from a mother who pumped when her baby was around that same age. However, as per the World Health Organization's guidelines, in most circumstances human milk is preferable to milk substitutes, even when there is a difference in age.
Q: Do I have to use a bottle to feed my baby donor milk?
A: No, many mothers use an at-the-breast supplementer to feed their babies. This device includes a container attached to a small feeding tube that is either taped to the breast or placed inside the baby's mouth while the baby is latched onto the breast. This allows the baby to receive the donor milk while still stimulating mother's breast and taking in any milk she is making. While this device can be purchased, you can also make your own. Some families use a small cup, a dental syringe, a spoon or other methods.
Tuesday, 22 November 2011
Our Pre-op Day
Wow that was a long day!!!
We had to arrive at the hospital at 7:30 a.m. Thank GOD for Tim Hortons in the hospital. Poor James had to be put into an x-ray tube, let me tell you he was not a happy Camper, DH could hear him screaming out in the waiting area. Poor little monkey was stuffed into something like this
Then we headed up to the Cardiac Unit to meet with our Pre-op Nurse. We had to fill out paperwork on James' History. The form we had to fill out is used for all patients from age 0 to age 18. I had a little chuckle when I answered the question "Does your child smoke" and Could you child be Pregnant.
We met with a surgical fellow who explained everything they would be doing. We met the surgeon who went over everything again and answered all the questions that had come up after talking to the fellow.
We then met the anesthesiologist who we LOVED!! But this is where I started to break down. The part of the whole surgery day that scares me the most is having to hand James over to the surgical team. We found out today that from the time we hand him over to the time he is asleep is only going to be 5 - 10 minutes which made me feel so much better!! I was afraid he was going to be awake and without us for longer.
We then found out the Pre-op blood work we did a few weeks ago need to be re-done because it contained blood clots. So back down to the outpatient lab we went.
After the blood work we met back up with the Nurse and took a tour of the unit James is staying on, and went over everything we need to pack, what to expect. They showed us pictures of what James is going to look like with all the tubes and wires.
So now all we have to do is wait and avoid germs for the next 2 weeks.
We had to arrive at the hospital at 7:30 a.m. Thank GOD for Tim Hortons in the hospital. Poor James had to be put into an x-ray tube, let me tell you he was not a happy Camper, DH could hear him screaming out in the waiting area. Poor little monkey was stuffed into something like this
 |
| Image from blowery.org |
Then we headed up to the Cardiac Unit to meet with our Pre-op Nurse. We had to fill out paperwork on James' History. The form we had to fill out is used for all patients from age 0 to age 18. I had a little chuckle when I answered the question "Does your child smoke" and Could you child be Pregnant.
We met with a surgical fellow who explained everything they would be doing. We met the surgeon who went over everything again and answered all the questions that had come up after talking to the fellow.
We then met the anesthesiologist who we LOVED!! But this is where I started to break down. The part of the whole surgery day that scares me the most is having to hand James over to the surgical team. We found out today that from the time we hand him over to the time he is asleep is only going to be 5 - 10 minutes which made me feel so much better!! I was afraid he was going to be awake and without us for longer.
We then found out the Pre-op blood work we did a few weeks ago need to be re-done because it contained blood clots. So back down to the outpatient lab we went.
After the blood work we met back up with the Nurse and took a tour of the unit James is staying on, and went over everything we need to pack, what to expect. They showed us pictures of what James is going to look like with all the tubes and wires.
So now all we have to do is wait and avoid germs for the next 2 weeks.
Monday, 21 November 2011
Sunday, 2 October 2011
Wednesday, 21 September 2011
My Heart Defect
I have a heart defect called Tetralogy of Fallot.
Here is information from the Child Heart Associates Tetralogy of Fallot (TOF) is one of the most common types of heart disease in children requiring surgical repair. It consists of a large hole between the two pumping chambers of the heart (ventricular septal defect, or VSD) and a tightening of the area leading out of the heart to the lungs (subvalvar pulmonary stenosis). The rest of the tetralogy ("four findings") don't make much sense to non-physicians as they are really anatomic details: an overriding aorta, and thickening of the right ventricle. Curiously, tetralogy of Fallot was not actually discovered by Etienne-Louis Arthur Fallot, but it was named for him because of a very good paper he wrote about it in 1888. It was actually first described by a fellow named Stinson. Although there are some more serious forms of TOF (including TOF with pulmonary atresia, TOF with absent pulmonary valve and TOF with other complex heart disease), most children with TOF do not have very much pulmonary stenosis at birth, and may be completely pink with no symptoms at all during the first few months of life ("pink tetralogy"). However, the pulmonary stenosis tends to gradually become worse over time, and most children will eventually become somewhat blue (cyanotic), due to blue (low oxygen) blood mixing with the pink (high oxygen) blood within the heart. Children can be cyanotic from birth, or can develop cyanosis gradually over time, usually within the first year of life. Because of the tendency for children to develop cyanosis, tetralogy of Fallot is often classified as a type of "cyanotic heart disease". There are many different types of cyanotic heart disease, however, most of which are far more severe than tetralogy of Fallot, so this is not a very useful term. Starting at about 6 months of age (occasionally sooner), a child with the usual type of TOF may start to have "tetralogy spells" ("tet spells" or "hypercyanotic spells"). Tetralogy spells can be triggered by anger, pain, feedings, a bath or even just waking up from a nap. During a spell, a child becomes short of breath, deeply cyanotic (with very low oxygen levels), irritable and even lethargic or unconscious. The first step in treating a child having a tetralogy spell is to place him or her in a fetal (knee-chest) position and keep them calm and comfortable. Although children most often will come out of a tetralogy spell on their own, tetralogy spells can be a real medical emergency. Generally it's best to call an ambulance right away unless a physician has specifically instructed otherwise. There are medications that can reduce the risk of tetralogy spells, but because of their side effects they are often not used unless a child has spells at an earlier age than usual, or develops spells before surgery is scheduled. Prior to surgical repair, children with tetralogy of Fallot must have a careful evaluation to outline all the details of their condition. Some children may have an abnormal artery supplying the heart itself with blood (conus coronary supplying the left anterior descending artery), additional holes between the pumping chambers, or abnormalities in the shape of the arteries to the lungs, any of which might require a different type of surgery, or surgery at a different age. Some centers obtain this information by performing an echocardiogram (ultrasound of the heart) and a cardiac catheterization, while others may perform only an echocardiogram. In addition, a fraction of children with tetralogy of Fallot also have a genetic condition known as DiGeorge syndrome or velocardiofacial syndrome, related to a mutation on chromosome 22. Surgical repair is required in every child with the usual type of tetralogy of Fallot, unless such a procedure would carry too high a risk for some reason. Because tetralogy spells can be dangerous, most cardiologists would recommend surgical repair within the first six months of life. In addition, there is evidence that waiting for surgical repair until after a year of age can increase the risk of serious cardiac complications, including abnormal heart rhythms, later in life. For other types of tetralogy of Fallot (listed above), surgery may be required earlier or later, or may not be possible at all. In the hands of a surgeon with a lot of experience in pediatric heart surgery, the surgical repair of tetralogy of Fallot is fairly low-risk, although of course all heart surgery entails some risk. Following surgical repair, it is reasonable to expect that children will have normal heart function and probably a normal life expectancy. We really don't know this for certain, however, as infant heart surgery has only been available for a few decades. On the other hand, children with tetralogy of Fallot who do not have surgical repair are very likely to have serious heart problems by early adulthood, and in most cases probably would have substantially reduced exercise tolerance, a low quality of life with frequent hospitalizations, and a significantly shorter life expectancy than other people. Approximately 40% of untreated patients with TOF die within the first 4 years of life, 70% by 10 years, and 95% by 40 years. For this reason, given what we know, surgical repair is the only sensible option.
 |
| image from Paramedicine 101 |
A busy week!!
Well we have not been around lately because we have been out and about visiting!! In the last 7 days I have only slept in my own bed twice.
Here is what we have been up to in pictures
I attended my first wedding
Me and Mom

A ladies Man, I picked up two older women!!

I took our first trip over the border to visit our American Friends

Big Tree Volunteer Fire Companies Newest Recruit

We came home then headed off on my second road trip:
A Canadian Road Trip Staple

Hanging in the Hammock

the view from our Hammock

And then back to the Camper and the Race Track to watch the Race Cars!!

Here is what we have been up to in pictures
I attended my first wedding
Me and Mom

A ladies Man, I picked up two older women!!

I took our first trip over the border to visit our American Friends

Big Tree Volunteer Fire Companies Newest Recruit

We came home then headed off on my second road trip:
A Canadian Road Trip Staple

Hanging in the Hammock

the view from our Hammock

And then back to the Camper and the Race Track to watch the Race Cars!!

Tuesday, 30 August 2011
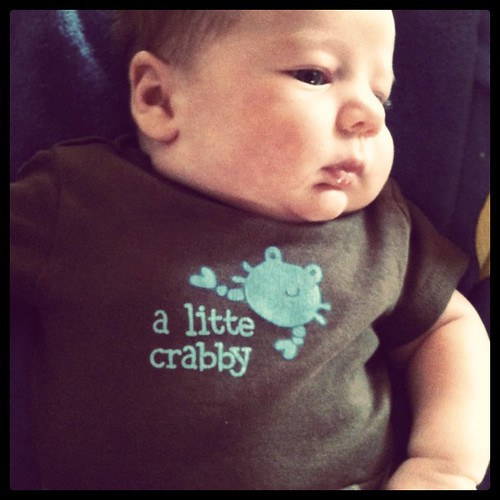
I am crabby
I have been very crabby lately and giving my mommy and daddy a run for their money.
This week I have to go to the Hospital for Sick Kids for an Echocardiogram.
I have been very busy, I attended two BBQs last weekend, and this weekend I am going to my first wedding and then a BBQ in my honor the next day!!
This week I have to go to the Hospital for Sick Kids for an Echocardiogram.
I have been very busy, I attended two BBQs last weekend, and this weekend I am going to my first wedding and then a BBQ in my honor the next day!!
Wednesday, 17 August 2011
Subscribe to:
Posts (Atom)